Recomendaciones Interinstitucionales Para Prevenir COVID-19 en Personal de Salud en Casos Sospechosos o Confirmados Por SARS-CO V2

Por el Consejo de Emergencias Cardiovasculares y Cardiología Crítica
La situación de pandemia por el coronavirus SARS-CoV-2 es algo que no será ajeno al mundo de la cardiología. Por esto creemos importante que conozcamos los mejores métodos para protegernos de un contagio.
La infección por SARS-CoV-2 se produce por vehiculización viral mediante gotas respiratorias producidas por la tos y /o estornudo así como por medio de contacto con superficies contaminadas producto de las mismas, la cual juega un rol primordial en la transmisión puesto que permanece con capacidad infectiva hasta 3 días dependiendo del material contaminado (3).
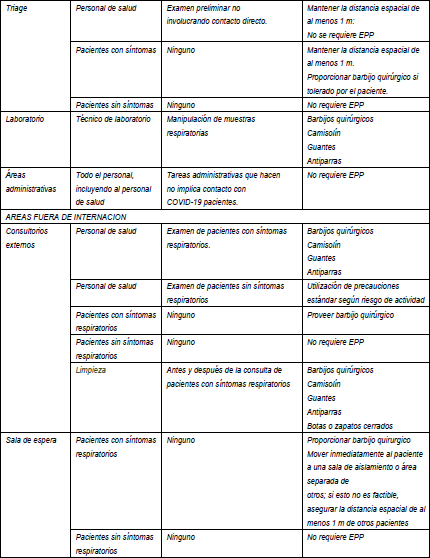
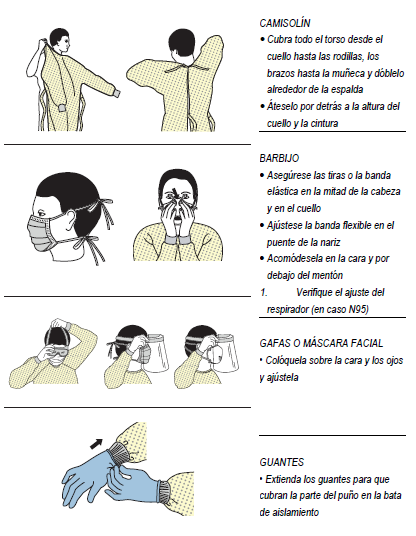
En el inicio epidémico en Whuan cerca de la mitad de los casos descriptos inicialmente correspondían a personal de salud (PS). Los elementos de protección personal (EPP) se utilizan para proteger al PS, asi como a los pacientes de infectarse o prevenir que infecten a otros.
ESTRATEGIAS
-
MODIFICACIONES EDILICIAS
Reducen la exposición del PS mediante la aplicación de barreras físicas entre la noxa y el PS. Entre ellas se encuentran, salas de aislamiento respiratorio barreras físicas: ventanas de vidrio/ plástico, sistemas de ventilación con dirección del aire del área limpia a la contaminada.
-
CONTROLES ADMINISTRATIVOS
Son políticas y prácticas laborales que minimizan o previenen la exposición. Incluyen agrupar por casos sospechosos, confirmados, suspender visitas, etc.
-
IMPLEMENTACIÓN DEL EQUIPO DE PROTECCIÓN PERSONAL (EPP)
Involucra un elevado nivel de entrenamiento.
EQUIPO DE PROTECCIÓN PERSONAL EN COVID-19
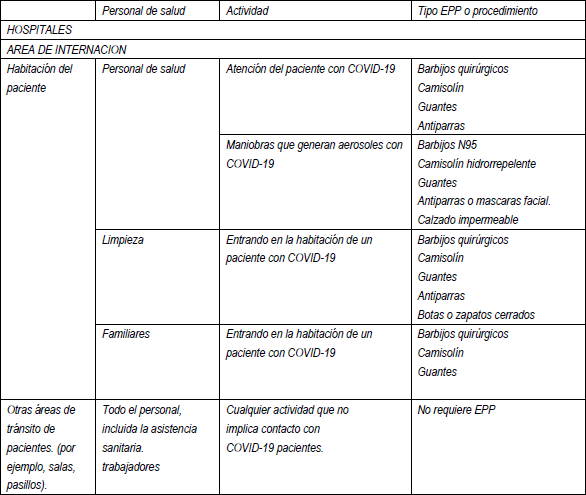
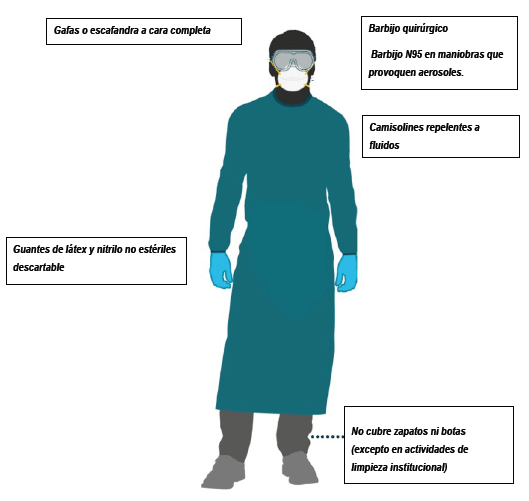
- El PS debe utilizar frente a caso sospechoso o confirmado: Guantes descartables (no estériles), camisolín, barbijo quirúrgico y protector ocular o un protector facial. Ver secuencia de colocación y retiro (9) (Recomendación IIa).
- El individuo que resulta casos sospechoso o confirmado: barbijo quirúrgico al salir de la habitación o traslado en el hospital. (9) (Recomensación IIa).
- Entre las personas con Infección respiratoria aguda (IRA): fomentar la higiene respiratoria (es decir, en caso del paciente sea capaz de comprender y realiza la maniobra, cubrirse la boca y la nariz al toser o estornudar, pañuelo de papel, la manga o el codo flexionado, asi como complementar con barbijo quirúrgico, sobre todo en pacientes sin capacidad de cumplir las pautas) y luego llevar a cabo la higiene de las manos para disminuir la dispersión de secreciones respiratorias que puedan contener partículas infecciosas.
- Mantenga la separación espacial (distancia mínima de 1 metro) entre cada paciente con infección respiratoria aguda y las demás personas, incluidos los profesionales de salud (sin equipo de protección personal), a fin de disminuir la transmisión de la infección.
- Vacune a los trabajadores sanitarios que atienden a los pacientes con alto riesgo de influenza.
- Gestione la cantidad suficiente y la continuidad de los insumos para para la prevención y el control de las infecciones (10)(11), por ejemplo: Dispositivos para la higiene de las manos ( jabón y agua corriente, desinfectante con base de alcohol para las manos y toallas de papel o de uso único)(2); Equipos de protección personal para atender al paciente (barbijos, camisolín, guantes y protección ocular) (2); Equipos de protección personal para la limpieza y recolección de residuos (calzado cerrado e impermeable, delantales impermeables y guantes de resistentes )(2),
- Personal de salud en contacto con un paciente con infección confirmada por COVID-19 que desarrolla fiebre o síntomas respiratorios, realizar la prueba de reacción en cadena de la polimerasa (PCR) para diagnóstico. Se recomienda la internación para seguimiento y control.
- Personal de salud asintomático en contacto estrecho con un paciente con infección confirmada por COVID-19 sin equipo de protección adecuado se podría indicar profilaxis post exposición con Lopinavir/Ritonavir según recomendación de expertos de SADI. Autoaislamiento domiciliario, seguimiento y control.
- El EPP para la atención de los pacientes con síndromes de infección respiratoria aguda puede incluir una combinación de los siguientes componentes: barbijos (quirúrgica o N95); guantes; camisolín de manga larga, y protección ocular (gafas de protección o protectores faciales).
- Procedimientos que generan aerosoles y que se asocian sistemáticamente con mayor riesgo de transmisión de agentes patógenos que causan infecciones respiratorias agudas, use guantes, camisolín de manga larga hidrorepelente, protección ocular (o máscaras faciales) y barbijo N95. Las pruebas muestran que la intubación endotraqueal o la exposición a ella, ya sea solo ese procedimiento o en combinación con otros (como la reanimación cardiopulmonar o la broncoscopia), se asocia con mayor riesgo de transmisión.
- Use los barbijos quirúrgicos bien ajustados a la cara y deséchelos de inmediato después de su uso. Cuando el barbijo se moja o se ensucia con secreciones debe cambiarse de inmediato. El uso del barbijo no debe exceder 1 hora y siempre que el barbijo no se haya humedecido o manchado.
- La máscara N95 es de uso prioritario para el personal de salud que atienda enfermedades de transmisión aérea o preferencial en el caso de procedimientos que generan aerosoles ya que tienen mayor riesgo de transmisión de agentes patógenos.(9)(12) En situación de pandemia, las máscaras N95 pueden ser de uso extendido (no mayor a 8 horas corridas ) y reutilizable.
- Antiparras o protectores faciales: para prevenir la exposición de la mucosa ocular al virus. Uso múltiple, exclusivo y se desinfecta después de cada uso.
- La ropa que utiliza el equipo de salud que atiende a pacientes con sospecha o confirmación de deberá ser exclusiva para el uso durante la guardia. Se prohibe la circulacion de personal de salud fuera del hospital con ambos y guardapolvos. Si la ropa se lava en el domicilio se debe trasladar en una bolsa cerrada y utilizar detergentes habituales y temperatura de 40 a 60 °C.
- Para la toma de muestra de hisopado nasofaríngeo se debe utilizar EPP con barbijo N95.
- Bibliografía
1. Xu Y, Li X, Zhu B, Liang H, Fang C, Gong Y, et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. 2019;
2. Ong SWX, Yian Kim T, Chia PY, Lee TH, Ng OT, Wong MSY, et al. Air, Surface Environmental, and Personal Protective Equipment Contamination by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) From a Symptomatic Patient. JAMA [Internet]. 2020;3–5. Available from: https://jamanetwork.com/journals/jama/fullarticle/2762692
3. Lloyd-smith JO, Munster VJ, Doremalen N Van, Bushmaker T, Morris DH, Myndi G, et al. Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1 Short author list : 2020;
4. Chan JF, Yuan S, Kok K, To KK, Chu H, Yang J, et al. Articles A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission : a study of a family cluster. Lancet [Internet]. 2020;6736(20):1–10. Available from: http://dx.doi.org/10.1016/S0140-6736(20)30154-9
5. Wang D, Hu B, Peng CH, Zhu F, Zhiyong, Wang X, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA. 2020;1–9.
6. Offeddu V, Yung CF, Low MSF, Tam CC. Effectiveness of masks and respirators against respiratory infections in healthcare workers: a systematic review and meta-analysis. Clin Infect Dis. 2017;65:1934–42.
7. Radonovich LJ, Simberkoff MS, Bessesen MT, Brown AC, Cummings DAT, Gaydos CA, et al. N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel A Randomized Clinical Trial. JAMA. 2019;322(9):824–33.
8. Centers for Disease Control Prevention. Coronavirus Disease 2019 (COVID-19) Strategies for Optimizing the Supply of N95 Respirators. 2020;
9. Kim JY, Song JY, Yoon YK, Choi S, Song YG, Kim S, et al. Middle East Respiratory Syndrome Infection Control and Prevention Guideline for Healthcare Facilities. 2015;47(4):278–302.
10. World Health Organization. Infection prevention and control of epidemic- and pandemic-prone acute respiratory infections in health care. 2014;1–133.
11. Interim Infection Prevention and Control Precautions for Possible or Confirmed 2019 novel Coronavirus (2019 nCoV), Middle East Respiratory Syndrome Coronavirus (MERSCoV) and Avian Influenza A in Healthcare Settings. 2020;1–26.
12. Siegel JD, Rhinehart E, Jackson M, Brennan PJ, Bell M. 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. 2007;1–135.
13. Centers for Disease Control Prevention. Sequence for putting on and remove personal potective equipment (PPE).
14. European Centre for Disease Prevention and Control (ECDC). Guidance for wearing and removing personal protective equipment in healthcare settings for the the care of patients Target audience Suggested minimal PPE set. 2020;(February):1–13.
15. Europeprotective equipment in the treatment of infectious diseases of high consequence A tutorial for trainers in healthcare settings. 2014. 1–90 p.
16. World Health Organization. Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19). 2020;(February):1–7.
17. The USA Food and Drugs Administration. Surgical Mask and Gown Conservation Strategies – Letter to Healthcare Providers. 2020;1–5.
18. Centers for Disease Control Prevention.The National Institute for Occupational Safety and Health (NIOSH). The National Institute for Occupational Safety and Health Recommended Guidance for Extended Use and Limited Reuse of N95 Filtering Facepiece Respirators in Healthcare Settings. 2020;1–6. Available from: https://www.cdc.gov/niosh/topics/hcwcontrols/recommendedguidanceextuse.html
19. Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect [Internet]. 2020;104(3):246–51. Available from: https://doi.org/10.1016/j.jhin.2020.01.022
20. Centers for Disease Control Prevention. Coronavirus Disease 2019 ( COVID-19 ) Environmental Cleaning and Disinfection Recommendations [Internet]. 2019. Available from: https://www.cdc.gov/coronavirus/2019-ncov/community/organizations/cleaning-disinfection.html
21. Centre for Health Protection Hong Kong. Infection Control Branch: Use N95 respirator properly. :1–3.
22. OPS-OMS. Requerimientos para uso de equipos de protección personal ( EPP ) para el nuevo coronavirus ( 2019-nCoV ) en establecimientos de salud. 2020;1–4.an Centre for Disease Prevention and Control (ECDC). Safe use of personal.








